Care for Back Discomfort Using Gentle Methods
Our care for back discomfort brings chiropractic, physiotherapy, and rehabilitation together to ease strain and improve function without injections or surgery. We focus on gentle, non-rotatory methods that assess posture, movement, muscle balance, and joint alignment, then guide you from “calm the flare” to “move with confidence.”
Because discomfort can start at different levels, we also outline segment-specific patterns from L1–L2 to L5–S1 and the tailbone how soft tissues, joints, discs, or pinched nerves may contribute, and how calm, careful progress helps. If stiffness, reduced function, or recurring strains are getting in the way, our integrated approach offers clear next steps delivered in plain language.
Whether you’re struggling with back stiffness, reduced function, or recurrent strains, CSC’s upper, mid and lower back techniques focus on comprehensive spine care.
Top 3 Essentials in Care for Back Discomfort (segment-aware)
- Segment-specific assessment: posture, movement, and palpation across L1–S1/tailbone to identify which level(s) are contributing then plan non-invasive care.
- Calm first, then build: gentle non-rotatory mobilization and movement re-education to settle the sensitive level(s), followed by core control that protects them
- Progress is reviewed at set checkpoints; staged rehabilitation continues as loading is reintroduced when the involved segment(s) tolerate it.
What a Gentle, Non-Rotatory Plan Looks Like (and when change is usually noticed)
Our plans start calm and precise no forceful twisting, no end-range cracking especially when inflammation is present.
How care begins (calm-first phase)
- Non-rotatory mobilization that targets the involved segment(s) in millimeter-level ranges.
- No deep paraspinal pressure over sensitive spots.
- Segment-specific methods chosen case-by-case, e.g.
-
- Flexion–distraction (brief, often under two minutes) to ease loading without rotation
- SOT blocks + Activator for gentle alignment cues.
- Angle-controlled decompression, high-intensity laser, ultrasound, focused shockwave at low settings when indicated always comfort-first.
- When movement is added: Only after the sensitive level(s) tolerate light contact without a spike. Introduce spine-neutral movement re-education and core control that protect L4–L5/L5–S1, progressing in small, testable steps.
- Checkpoints (not promises): Many people report steadier days within 2–4 weeks when flare drivers (sitting load, end-range bends, twisting) are reduced and loading is reintroduced gradually. We review progress at set checkpoints (e.g., visit 5, 10, 15) and adjust.
- How to choose a provider: Ask whether care is non-rotatory during inflammatory phases. Ask if they can provide flexion–distraction, SOT, Activator, and short, comfort-first applications rather than long or forceful sessions. Ensure they correlate exam findings with any available imaging before deciding on methods.
Educational guidance only. Follow a plan after a thorough assessment by a registered clinician.
What to do in a Flare: Positions, Cold vs Heat, and When to Seek Care
When symptoms surge, the goal is to decrease the irritation, making it quiet again, not “push through it.”
Positions
- Side-lying is usually best. Choose the side that feels least painful.
- Pillow between knees; a small pillow at the waist/low back to keep neutral.
- Log-roll to get in/out of bed.
- If (and only if) lying on your back is the least painful: calves on pillows/chair, spine neutral.
Activity
- Essentials only (bathroom/food) done gently.
- Avoid end-range stretches, twisting, deep tissue work, or self-“cracking.”
Cold vs heat
- During inflammatory phases, use cold packs (10–15 minutes with a thin towel barrier), several times daily if comfortable.
- Avoid heat in a flare; it may ramp irritability.
- Consider heat only when the source is a clear, isolated muscle spasm and no inflammatory signs are present confirm with your clinician first.
When to seek care promptly
- New/worsening leg weakness or foot drop
- Bowel or bladder changes
- Saddle numbness
- Fever or rapidly escalating pain
- Recent significant trauma
These home steps are general. Use them only after advice from a registered clinician who has examined you. During inflammatory phases, we avoid rotatory “cracking” methods; gentler options like flexion–distraction (brief), SOT, and Activator are typically better tolerated.
Contact Us for Care for Back Discomfort
If you’re ready to recover from back discomfort through integrative, non‑invasive care combining chiropractic, physiotherapy, and rehabilitation in a gentle, non‑rotatory spine and joint center, contact us today to arrange a personalized evaluation: Contact us
Segment-Specific Back Discomfort (L1-L2 → L5-S1 & Tailbone)
Back discomfort may arise from soft tissues, joints, discs, or pinched nerves. Below are common patterns seen at each level (guidance only individuals vary):
L1-L2 (upper lumbar)
- Often linked with front-of-hip/groin ache or upper-thigh tension
- Typical issues: disc changes, small-joint irritation, hip-flexor strain
- May feel worse with long sitting or sudden trunk extension
L2-L3
- Front-thigh fatigue or tightness; sitting-to-stand stiffness
- Disc changes and joint irritation are common; quadriceps/iliotibial tension may show up
- Prolonged sitting or slumped posture can aggravate
L3-L4
- Ache around the knee/front-outer thigh; step-down/squat discomfort
- Disc changes, facet (small-joint) irritation, and muscle imbalance are frequent
- Often benefits from posture reset and segment-specific mobility (gentle, non-rotatory)
L4–L5 (high-load segment)
- Buttock/outer-leg discomfort; sitting and bending feel tight
- Common site for disc changes and joint irritation; recurrent strains are typical
- Core control and hip mechanics matter for this level
L5-S1 (lumbosacral junction)
- Low-central back with possible back-of-thigh tension
- Disc changes, sacral-base stress, and hamstring tightness are common drivers
- Prolonged flexed posture or heavy lifting can flare symptoms
Tailbone (coccyx)
- Pain with sitting on hard surfaces; sensitivity when leaning back
- Often related to falls, prolonged sitting, or pelvic-floor tension
- Cushioned sitting and gradual mobility are usually better tolerated
How To Recover From Your Back Discomfort Without Medication, Injections, Or Surgery?
Many have asked, What is the suitable method to Recover from back discomfort? As a result, we have prepared this article to answer that question. Back discomfort is the leading cause of disability for millions. It is the number one reason for emergency room visits and missed workdays. Before providing the answer to the question, let’s explore the primary reasons why back discomfort is becoming such a huge problem:
- We sit too long
- Lack of physical activity
- Neglecting a minor back issue
- Improper care
Why Sitting Is The Number One Cause Of Back Discomfort?
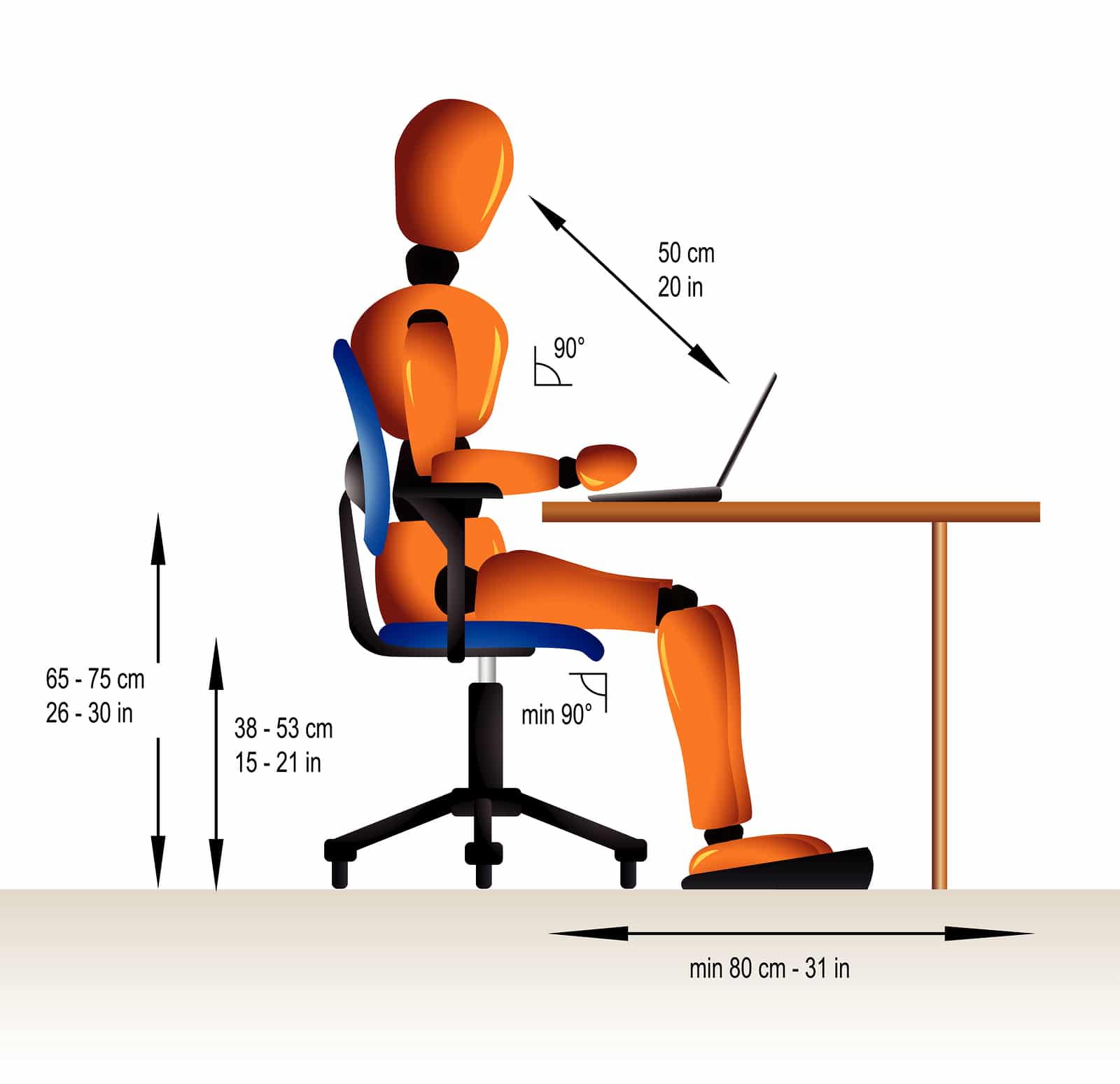
Pay attention to your posture if you want faster recovery. And should that fail, consider getting CSC’s targeted care for back discomfort. Prolonged sitting and poor sitting posture are the leading causes of back discomfort. In a seated position, the spinal disc is under excessive load. Anytime the spinal joints or spinal discs are under load, the pressures within discs and joints increase. The average intradiscal pressure (pressure inside spinal discs) in the supine position (lying on your back) is 25 mmHg.
Standing for prolonged periods can increase this pressure to 100 mmHg. Bending at the waist raises it to 150 mmHg. But sitting can increase the intradiscal pressure to 200 mmHg. And, leaning forward in a seated position can lead to intradiscal pressures of 250 mmHg or more. The increased pressures in joints and spinal discs during sitting positions lead to degenerative changes that are life-changing.
So, the first thing you would need to do is to be aware of your posture. This holds especially true if your job requires sitting. The worst sitting position is one that requires you to sit in front of a laptop. Those who use a computer regularly sit in a slightly flexed position. As such, these are individuals who experience more serious forms of back discomfort. Healing back discomfort is not possible unless poor posture is limited. You may not be able to avoid sitting, but you should pay attention to your sitting posture.
Don’t Neglect Minor Discomfort.
There is no such thing as a normal backache. So, if the discomfort you experience isn’t normal, shouldn’t you have it checked out? Of course, you should. It is always better to solve a simple problem than a complicated issue, such as a herniated disc, extruded disc, or fragmented disc. Back care needs to start as soon as you feel discomfort. You can initiate some of them at home. For starters, put an ice pack on for 15 minutes. Icing the back will reduce the swelling. But, make sure not to put the ice for more than 15 minutes, and never put ice directly on the skin. It would help if you used a towel. Between the ice pack and your skin. If the discomfort continues or emerges again, visit one of our centers.
Our advice to those who experience even the mildest back issue is to visit a Chiropractic Specialty Center® near you. If you live in Shah Alam, visit the recommended clinical chiropractic and physiotherapy team of experts in Kota Kemuning (Shah Alam) today. We can provide targeted care for back discomfort without injections or spine surgery.
Improper Care Of Mild Discomfort Leads To Complicated Back Issues
The Klang Valley has hundreds of competing centers claiming to offer successful therapies for back discomfort. However, the vast majority of them lack a basic understanding of identifying the actual cause of back discomfort. Identifying the cause through proper diagnosis is the first step toward recovery. Improper diagnosis is the leading reason for a failed recovery. Therefore, we encourage you to opt for focused care that addresses the actual cause of your discomfort.
Our clinical teams have the expertise, knowledge, and specialized technology that may help your recovery by addressing the root-causes of your discomfort. Holistic care of the spine through our integrated corrective methods of chiropractic and physiotherapy is a non-invasive option that is safe and gentle.
How To Recover From Back Discomfort Without Surgery?
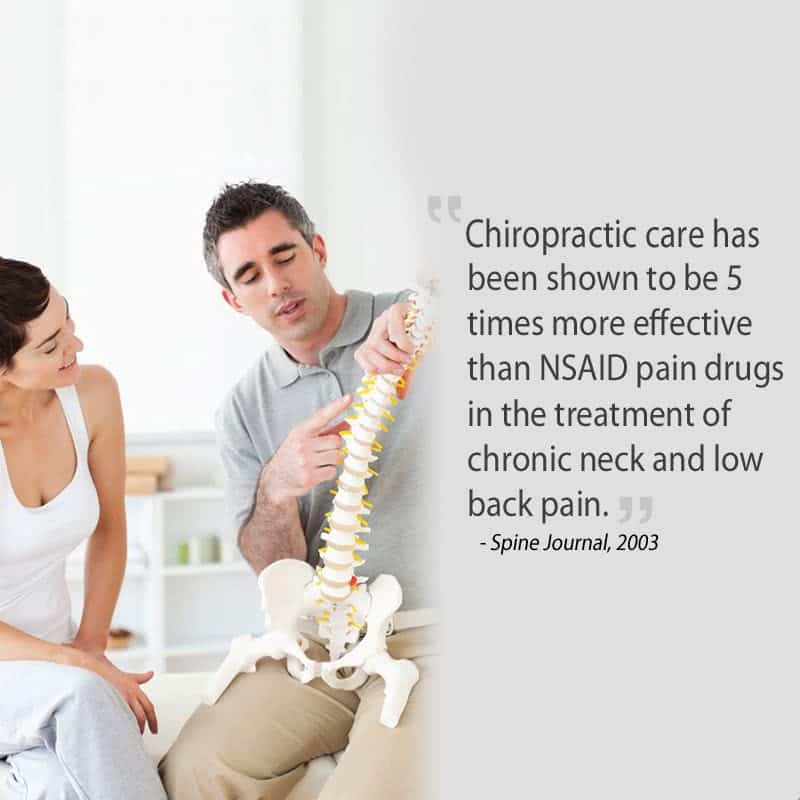
As mentioned, numerous centers manage back discomfort. The most functional of these centers are those that address patients collaboratively. In other words, chiropractic and physiotherapy are the well-known means of back care if you want to avoid spine surgery. However, the provided care must consider joint and spinal disc health before care. Chiropractic care that incorporates rotatory adjustments (manual adjustments with patients lying on their sides) tends to aggravate the joint. Yes, it feels great to get the spine cracked, but in particular instances, it can further irritate the joint capsule or spinal discs.
Gentle, Timing-Right Physiotherapy
Our approach is non-aggressive by design. In the early stage when joints, discs, or soft tissues are irritable forceful stretching, twisting, or high-pressure techniques can flare symptoms. We avoid end-range stretches, deep paraspinal pressure, and any maneuver that provokes pain. Care begins with calm, precise steps; mobility and strengthening are introduced only when tissues tolerate them.
- Heat vs. cold: Hot packs can feel soothing, but in an inflammatory flare they may increase irritability. We reserve heat for later phases and favor options that keep the area quiet in the beginning.
- Manual work: Deep myofascial release directly over the facets, spinous processes, or paraspinals can aggravate a sensitive back. We use light, comfortable contact and non-rotatory methods until the spine settles.
- Ultrasound technique: When ultrasound is used, it’s a dose-controlled modality not a pressure massage. The applicator glides smoothly on a continuous layer of gel with light, even contact (no scraping or pressing that squeezes out the gel). The goal is gentle energy delivery to the intended tissues, not mechanical force.
In short: Right care, right time. We first calm the area, then add movement re-education and progressive loading always pain-aware, always non-rotatory.
Let Our Clinical Teams Of Chiropractors & Physiotherapists Provide The Targeted Care You Need.
We can start a focused program that targets back issues with CSC’s targeted care for back discomfort without spine surgery. Our clinical integrative teams of chiropractors and physiotherapists in Kota Kemuning, Shah Alam have the expertise and the technology to provide precise care for back discomfort without spine surgery, injections, or medication. If you live in Klang or near Setia Alam, please contact our chiropractic & physiotherapy center in Setia Alam.
Chiropractic Specialty Center® in Shah Alam (Kota Kemuning & Setia Alam), Bukit Damansara, Petaling Jaya, and Sungai Buloh specializes in non-invasive clinical back care through non-surgical decompression therapy (NSD Therapy®). In our centers, we combine research-based chiropractic, clinical physiotherapy, modern spinal decompression, and target-specific rehabilitation with CSC’s focused care for back discomfort without neck surgery or back surgery.
NSD Therapy® method may help patients with back problems to recover non-invasively . If you are considering back surgery, you may want to take the initiative to seek a second opinion at CSC. Have one of our team members assess your back to see if our methods of care with or without NSD Therapy® is a right options before making your decision. Back surgery should always be the last option, as any surgical procedure comes with its own set of risks.
Chiropractors and physiotherapists at Chiropractic Specialty Center® have registered clinicians who can help you answer your questions and doubts. We have several locations throughout the Klang Valley. If you live in Shah Alam, Kuala Lumpur, Petaling Jaya, or Sungai Buloh, rest assured that our clinical teams can deliver the targeted non-surgical back care options for you.
Can Surgery Heal Or Cure Your Back Discomfort?
Surgery can help selected cases, but should be your last option. Symptoms may recur if other contributors aren’t addressed.
Consider a second opinion and non-invasive options when appropriate.” Consider a second opinion and non-invasive options when appropriate. Therefore, in our opinion, back surgery should be the absolute last resort. Moreover, our views regarding spine surgery are based on the research published by surgical and non-surgical experts.
The suitable thing you can do for your back discomfort is the non-invasive methods of care for back discomfort that we offer in our centers. So, before opting for invasive procedures, learn as much as you can. Life is too short to live with regrets.
What Are The Surgical Goals Of Spine Surgery?
The shared goal of surgery is to achieve decompression of a disc bulge, disc herniation, or disc extrusion. Surgical decompression removes the compressive effects by cutting the protruded, bulged, or herniated disc fibers. The problem with this procedure is that it does not address the cause of your spinal disc disorder. In other words, your back discomfort may have resulted from weak muscles, injured ligaments, irritated joints, and, of course, tears and slippage of spinal discs.
The surgical intervention only addresses one component, the slip of the protruded disc. They go in and cut those fibers. Some procedures may even involve the shaving of bones and spinal joints. The process of cutting protruded discs and shaving the bony landmarks of the spine in itself often leads to additional problems later in life.
Spinal joints and spinal discs are encapsulated structures, and an invasive procedure will alter the homeostasis of the spinal joint and spinal discs. Yes, it is possible to have a discomfort-free life for a while. The length of improvements is dependent on several factors, and it varies from person to person. Currently, published research puts this discomfort-free period anywhere from two to five years. And that is if your surgery is successful! The invasive nature of spine surgery and the harmful impact on the soft tissues (muscles and ligaments) are the primary reasons for the relapse of back discomfort. Also, there are scenarios where patients get worse after surgical intervention.
Complications and side effects of spine surgery are too numerous for us to address in this brief article, but can include increased discomfort, numbness in the legs, weakness in the legs, paralysis, or worse. There are several types of back surgery. We will discuss the three most common types of back surgery here.
Laminectomy
Laminectomy is a surgical procedure that involves the removal of the bony arch called the lamina. The lamina is an essential bone providing attachment points for muscles and a protective barrier for the spinal cord and nerves. Removal of the lamina leads to more serious spine issues later. The laminectomy process starts with the removal of the lamina, bone spurs (bony projections), muscles, and ligaments, leading to spinal instabilities. Spinal instabilities brought forth through laminectomy are a leading cause of disability.
Patients who opt for a laminectomy can experience acute discomfort for months or years following their surgery. Most complain of a recurrence of discomfort months or years post the operative procedures. In addition to laminectomy, some may also have a spinal fusion, which may further stress the healthy spinal segments. Spinal fusion can help stabilize the spinal segment in need of an operative intervention, but it places undue burdens on adjacent vertebrae. In time, the healthy vertebrae start showing signs of wear and tear. The wear and tear of the healthy vertebrae result from increased stresses resulting from the fusing of spinal bones.
Discectomy may be considered if conservative care is not sufficient.
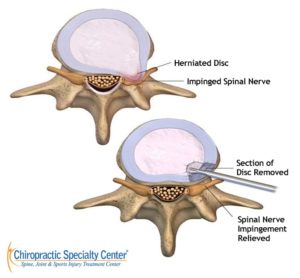
Discectomy is a procedure whereby parts or the entire intervertebral (IV) disc is surgically removed to relieve the area of nerve root compression. If only a part of the IV disc is removed, it is referred to as microdiscectomy, while removing the entire IV disc is called a discectomy. A microdiscectomy is a minor invasive procedure when compared to the traditional open back discectomy. However, this would entirely depend on the severity of the IV disc herniation, i.e., disc bulge, herniation, and extrusion.
Discectomy removes disc material that irritates a nerve; it does not address other contributors (e.g., joint, muscle, movement factors). Outcomes vary.
Apart from that, the recovery rate post-operation is lower in a microdiscectomy compared to a discectomy procedure. The downfall of microdiscectomy is that, in time, a relapse occurs, and such is the need for further surgical interventions. Therefore, a conservative course of care is better in the long term. But for conservative care to work, it must be targeted and based on an accurate diagnosis.
Spinal Fusion has Risks and Variable Outcomes!
Spinal fusion has meaningful risks and variable outcomes. Discuss potential benefits and trade-offs with your surgeon for your specific case.
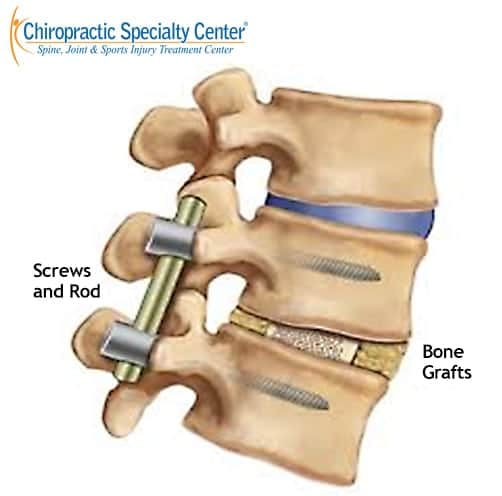
Spinal fusion is a surgical procedure performed to fuse or join two or more vertebrae. Typically, it is provided together or in combination with other surgical procedures such as discectomy. Spinal fusion can relieve some of the nerve root compression, but the loss of segment mobility often causes additional issues that were not present before.
Spine fusion is often performed on patients with hypertrophy of ligamentum flavum, spinal canal stenosis, or facet arthritis (facet hypertrophy). Some studies in selected populations report high rates of ongoing symptoms after fusion; estimates vary. Discuss expected outcomes for your specific case with your surgeon. Before you opt for a non-reversible operative procedure, contact us for recommended conservative care.
It is normal to feel worried or anxious when you are diagnosed with a bulging or a herniated disc. Ultimately, it is your decision. But, do take our advice and avoid spine surgery. You should exhaust your conservative care first before even thinking of getting surgery.
In a large study of workers’ compensation patients with chronic low back pain, people who had a lumbar fusion were less likely to return to work within two years (26% vs 67%), had more complications (36%), a high re-operation rate (27%), greater opioid use after surgery (76% still using; average daily use up 41%), and far more days off work than similar patients who didn’t have surgery. These results are from an observational cohort in a workers’ comp setting (not all patients), but they highlight why many individuals explore non-invasive options and second opinions before considering fusion. According to Nguyen and colleagues, published February 15, 2011, in Spine, see Ref number 7 below under citations.
NSD Therapy®: a gentle, team-based protocol for back discomfort

NSD Therapy® isn’t one machine or a single technique it’s a structured plan delivered by a chiropractor-physiotherapist team. The aim is simple: calm irritated tissues and improve movement without forceful methods.
How it works (in plain words):
- We start with a careful assessment of posture, movement, and segment sensitivity.
- Care begins gently to settle the area first; loading and exercises are added only when the back tolerates them.
- Depending on what you need, the plan may include angle-controlled spinal decompression, flexion-distraction, high-intensity laser (Class IV), therapeutic ultrasound, electrotherapy, focused shockwave at low settings for tender points, and segment-specific, non-rotatory chiropractic mobilization.
- Each step is comfort-first no twisting or deep pressure over sensitive spots.
Who may consider NSD Therapy®?
People with ongoing back discomfort that tends to flare, whether it feels local to the lower back or seems to travel toward the hips or legs. The protocol is designed to address common sources of irritation around discs, small spinal joints, and nearby soft tissues selected only after an individual evaluation.
What to expect:
Short sessions that stay within a comfortable range, clear checkpoints to review progress, and guidance on everyday movements as things settle.
If you’d like to find out whether NSD Therapy® is suitable for you, book a personalized evaluation at a nearby CSC center. We’ll review your findings together and discuss the non-invasive options that fit your situation.
Author Information
Yama Zafer, D.C. – Care for Back Discomfort | Gentle Chiropractic & Physiotherapy – CSC: Was written by Yama Zafer, D.C., educational background in physiotherapy and chiropractic from Cleveland Chiropractic University, Kansas City, with nearly 30 years in physiotherapy and chiropractic non‑invasive care. Read more about Y. Zafer on his official bio page.
Peer‑Reviewed References
- McKenzie RA. The Lumbar Spine: Mechanical Diagnosis and Therapy. Spinal Publications; 1981.
- Ferreira PH, et al. Specific stabilisation exercise for spinal and pelvic pain in pregnancy. Cochrane Database Syst Rev. 2013;(12):CD009225.
- Rubinstein SM, et al. Spinal manipulative therapy for chronic low back pain. Cochrane Database Syst Rev. 2011;(2):CD008112.
- Hides JA, et al. The relationship of trunk muscle function to low back disorders. J Orthop Res. 2008;26(3):414–419.
- O’Sullivan PB. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10(4):242–255.
- Saragiotto BT, et al. Motor control exercise for chronic non-specific low-back pain. Eur Spine J. 2016;25(6):1924–1940.
- Nguyen TH, Randolph DC, Talmage J, Succop P, Travis R. Long-term outcomes of lumbar fusion among workers’ compensation subjects: a historical cohort study. Spine (Phila Pa 1976). 2011;36(4):320-331.
Last Updated
Was last revised and updated by Y.Zafer, D.C. on September 1, 2025 – Care for back discomfort using gentle methods
FAQs: Back Discomfort (Practical Answers)
Back discomfort can start in soft tissues, small joints, discs, or nearby nerves. Patterns differ by level:
L1–L2: front-of-hip/groin tightness; sitting upright or sudden extension may irritate.
L2–L3: front-thigh fatigue or stiffness rising from a chair; prolonged sitting can flare.
L3–L4: knee/front-outer thigh ache; step-downs or deep bends feel restricted.
L4–L5: buttock/outer-leg tension; bending and long sitting feel tight.
L5–S1: low-central back with back-of-thigh pull; heavy lifts or slumped posture aggravate.
Tailbone (coccyx): pain on hard chairs or leaning back; often after prolonged sitting or a fall.
How we use this: your history and movement screen highlight which segment(s) are sensitive so care for back discomfort can be targeted and non-invasive.
We start with a segment-specific assessment (posture, movement, palpation; review of existing imaging if available). Care for back discomfort begins with a calm-first phase—no twisting, no deep pressure over sensitive spots. Depending on your findings, your plan may include non-rotatory mobilization, clinician-directed modalities (e.g., carefully dosed laser, ultrasound, or focused shockwave at low settings for tender points), and spine-neutral movement re-education. As irritability settles, we add core control and graded loading that your segment(s) can tolerate without flare-ups.
Typical timelines: some people notice steadier days in 2–4 weeks when flare-drivers (posture, sitting load, end-range bends) are managed early. Progress is reviewed at set checkpoints; plans are adjusted based on response.
During a hot phase, the goal is to quiet things down:
Positioning: side-lying is usually best; choose the side that’s least painful. Pillow between knees; small pillow at the waist/low back. Log-roll in/out of bed.
Activity: essentials only (bathroom/food) done gently. Avoid end-range twists, deep stretches, or “cracking” maneuvers.
Cold packs: 10–15 minutes with a thin towel barrier, several times a day; stop if it aggravates.
When symptoms cool, your clinician will guide gradual mobility and strengthening that do not spike the sensitive segment(s).
Seek urgent care if you notice new or worsening leg weakness, bowel or bladder changes, saddle numbness, fever,or rapidly escalating pain.

