Plantar Fasciitis Guide for Foot & Heel Care
Plantar fasciitis and heel spurs can cause persistent foot discomfort, often affecting mobility and daily activities. At Chiropractic Specialty Center® (CSC), a non-invasive, evidence-based approach is used to manage these conditions without the need for surgery or injections. By combining chiropractic care, physiotherapy, and integrated therapy modalities, CSC provides targeted solutions that address the root causes of foot discomfort rather than just managing symptoms.
The structured approach at CSC includes manual therapy, ultrasound, shockwave therapy, high-intensity laser therapy (HILT), and chiropractic adjustments to help tissue recovery, improve foot function, and enhance overall mobility. In addition to hands-on techniques, custom orthotics and proper footwear recommendations help maintain long-term foot stability.
Many individuals experiencing plantar fasciitis can benefit from lifestyle adjustments, including stretching exercises, proper footwear selection, and reducing excessive strain on the plantar fascia. For those at risk, such as individuals with flat feet, high arches, or prolonged standing jobs, taking proactive measures can help prevent foot-related discomfort.
By utilizing a patient-centered, non-surgical foot and heel approach, CSC focuses on long-term recovery and foot health rather than temporary relief. If symptoms persist despite home care efforts, professional evaluation and structured rehabilitation may provide the necessary care to restore function and alleviate discomfort.
Key Takeaways for Plantar Fasciitis
- Plantar Fasciitis is often caused by strain on the plantar fascia due to tight muscles, poor posture, or improper footwear.
- Chiropractic, physiotherapy, and rehabilitation at CSC provide non-invasive care tailored to your foot’s mechanics and walking pattern.
- Early action with custom stretching, footwear advice, and gait correction can improve alignment and reduce long-term discomfort.
Contact Us to Book a Plantar Fasciitis Evaluation
Get in touch with us today to schedule your plantar fasciitis assessment. Our team will evaluate your foot alignment, walking pattern, joint health, and muscle tension through a non-invasive chiropractic, physiotherapy, and rehabilitation approach. Start your foot care journey by visiting our Contact Us page.
Plantar Fasciitis Physiotherapy & Chiropractic Care in KL
At Chiropractic Specialty Center® in Kuala Lumpur, we deliver advanced, non-surgical plantar fasciitis care through a structured integration of physiotherapy, chiropractic, and rehabilitative techniques. Rather than masking symptoms, our approach addresses the root biomechanical and tissue-level causes of heel and arch discomfort safely and precisely.
Each session begins with a comprehensive foot assessment, analyzing plantar tension, arch integrity, and weight distribution. Shockwave therapy is applied to promote regeneration in chronically strained fascia, triggering natural healing responses at the cellular level. High-intensity laser therapy then penetrates deeper soft tissues to accelerate circulation, oxygen delivery, and collagen synthesis key factors in long-term recovery.
Underwater ultrasound therapy, a rare modality in KL, is used to deliver targeted acoustic waves in a water medium enhancing depth while minimizing surface irritation. Electrotherapy further supports neuromuscular reconditioning and fascial responsiveness, especially where heel fatigue has persisted for months.
Manual care focuses on myofascial release and trigger point therapy, easing pressure in the calf-arch complex and restoring balance along the plantar line. For joint alignment, we use the Activator Method, a gentle, instrument-based chiropractic technique ideal for correcting dysfunctions in the navicular, talus, and metatarsals without twisting or high-force movements.
Our heel and arch rehabilitation programs include towel curls, resisted toe flexion, balance board work, and progressive loading drills customized to your structure and movement goals. This integrative method promotes stable recovery, gait correction, and lasting improvements without surgery or steroid injections.
Plantar Fasciitis Care In All Kuala Lumpur’s Neighborhoods by CSC 3 KL based Centers
CSC provides targeted plantar fasciitis physiotherapy and chiropractic care in KL to residents of Bukit Damansara, Mont Kiara, Bangsar, TTDI, Sri Hartamas, Sri Petaling, Bukit Jalil, Bandar Sri Damansara, and Kepong. Sessions are one-on-one and led by certified practitioners.
References – Evidence Supporting Plantar Fasciitis, Heel & Arch Rehabilitation
- Speed C. (2014). A systematic review of shockwave therapy for plantar fasciopathy. Br J Sports Med, 48(21), 1538–1542.
- Kiritsi O, et al. (2010). Effectiveness of high-intensity laser therapy in plantar fasciitis. Photomed Laser Surg, 28(1), 103–108.
- Galletti R, et al. (2017). Efficacy of underwater ultrasound in musculoskeletal rehabilitation. Eur J Phys Rehabil Med, 53(2), 188–193.
- Cotchett MP, et al. (2015). Trigger point therapy for plantar heel pain: a randomized controlled trial. J Orthop Sports Phys Ther, 45(8), 582–590.
- Landorf KB, et al. (2006). Effectiveness of foot orthoses and physical therapy for plantar fasciitis. Arch Intern Med, 166(12), 1305–1310.
Understanding Plantar Fasciitis and Foot Health
Plantar fasciitis is a common foot condition that arises due to weakness in the foot muscles and ligaments, affecting the plantar fascia a thick tissue band that manages the foot’s arch. This connective tissue plays a crucial role in absorbing shock and maintaining stability, but when foot muscles weaken, excess strain is placed on the plantar fascia, potentially leading to discomfort.
One contributing factor to weakened foot muscles is the consistent use of rigid or overly cushioned shoes, which limit natural foot movement. The foot consists of four layers of muscles that work together to help with daily activities. Reduced engagement of these muscles over time can lead to muscle imbalances, increasing the risk of plantar fasciitis and heel-related concerns.
Flat arches or overpronation, where the foot rolls inward excessively, can further contribute to plantar fascia tension. This strain typically originates at the heel and extends toward the toes, leading to discomfort, particularly during the first steps in the morning. To counteract these issues, incorporating strengthening exercises for the foot, such as toe curls or picking up small objects with the toes, can help rebuild muscle guide and stability. Additionally, choosing footwear that promotes natural movement and offers proper arch structure can help maintain foot comfort and function
Plantar fasciitis is not solely a ligament issue; it often results from weak foot muscles and improper footwear choices. Making simple lifestyle adjustments, such as strengthening exercises and proper footwear selection, can assist in maintaining overall foot function and reducing strain over time
What Is Plantar Fasciitis?
Plantar fasciitis is a common condition affecting the plantar fascia, the connective tissue that runs along the bottom of the foot. This structure connects the heel bone to the toes and plays a vital role in managing the foot’s arch.
When the plantar fascia becomes strained or inflamed, it can result in heel and foot discomfort, which can significantly impact daily mobility and quality of life.
How CSC Enhances Recovery from Plantar Fasciitis
At Chiropractic Specialty Center® (CSC), a structured, individualized approach is taken to address plantar fasciitis in Kuala Lumpur. A thorough foot assessment and lifestyle evaluation are conducted to identify contributing factors, such as prolonged use of rigid-soled shoes, which may weaken the foot’s muscles and ligaments. Over time, this can lead to subtle misalignments in the 28 interconnected bones of the foot, contributing to plantar fasciitis.
The approach focuses not just on symptom relief but on addressing the root causes of plantar fascia discomfort. Diagnostic imaging may be used when necessary to identify issues such as dropped arches or heel spurs, allowing for the creation of a personalized recovery plan.
Combining Foot Physiotherapy and Chiropractic Care for Heel, Muscle, and Plantar Fascia Guide
CSC integrates chiropractic foot care with targeted physiotherapy techniques to manage plantar fascia concerns efficiently. Some of the specialized methods include:
- Shockwave Therapy – Helps break down adhesions and scar tissue, managing tissue mobility.
- Ultrasound Therapy – Promotes circulation and soft tissue healing.
- High-Intensity Laser Therapy (HILT) – Works in combination with shockwave and ultrasound therapy to help reduce inflammation and enhance tissue repair.
These therapeutic methods extend beyond the plantar fascia, addressing the arches and joints of the foot, including the navicular, cuboid, and metatarsals, which may be affected by plantar fasciitis. Additionally, targeted exercises and stretches are incorporated to strengthen the foot’s layered muscles, enhancing overall stability and function.
By addressing both the underlying causes and functional limitations, CSC provides comprehensive care to restore proper foot movement and reduce the likelihood of recurring issues.
Understanding the Plantar Fascia and Its Role in Recovery
The plantar fascia is a thin, strong band of connective tissue that plays a crucial role in providing help and stability to the foot. Located just beneath the skin, it extends from the heel bone (calcaneus) to the ball of the foot and toes.
Individuals can feel the plantar fascia by gently pulling back their toes the rope-like structure in the center of the foot is the plantar fascia. Understanding its function can help individuals make better decisions regarding foot care and recovery strategies.
Understanding the Function of the Plantar Fascia
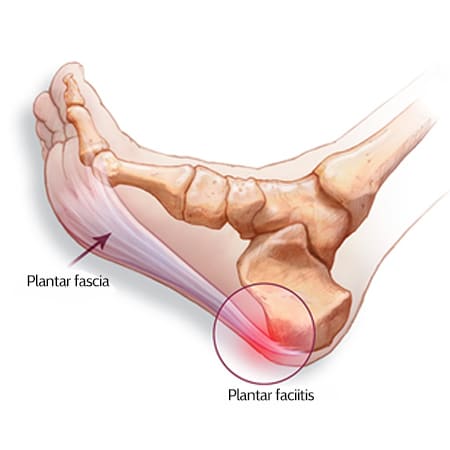
The plantar fascia plays a crucial role in managing the foot’s arch and ensuring proper weight distribution during standing and walking. This connective tissue functions as a shock absorber, helping to stabilize the foot during movement and preventing excessive strain on specific areas.
Key Roles of the Plantar Fascia:
- Distributes Body Weight – Ensures even weight distribution to prevent excess stress on certain parts of the foot.
- Maintains Arch Stability – Helps keep the foot’s arch managed during standing, walking, or high-impact activities.
When excessive stress is placed on the plantar fascia due to repetitive movements or prolonged strain, micro-tears may develop, increasing the risk of plantar fasciitis.
How Plantar Fasciitis Develops
Plantar fasciitis occurs when the plantar fascia becomes inflamed or irritated due to prolonged strain. This condition typically involves micro-tears where the fascia attaches to the heel bone or along areas of tension on the sole.
Common Factors Contributing to Plantar Fasciitis:
- Increased Body Weight – Excess weight may place additional pressure on the foot ligaments.
- Improper Footwear – Shoes with minimal arch cushioning can prevent proper weight distribution, leading to excess strain.
- Prolonged Standing or Repetitive Impact – Engaging in activities that involve extended standing, walking, or repetitive strain can contribute to plantar fascia irritation.
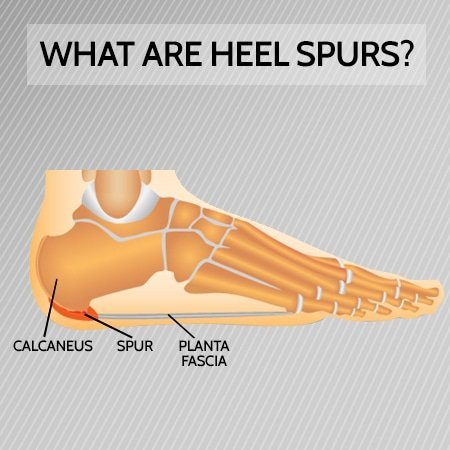
If left unmanaged, chronic plantar fasciitis may lead to the formation of heel spurs, which can exacerbate symptoms and prolong recovery.
Recognizing the Symptoms of an Inflamed Plantar Fascia
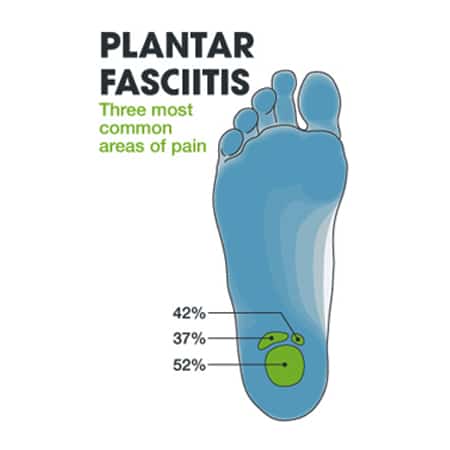
Plantar fasciitis often presents with discomfort concentrated near the heel. Some of the most common symptoms include:
- Sharp or Stabbing Sensations – Typically felt during the first steps in the morning or after prolonged rest.
- Activity-Triggered Discomfort – Symptoms may worsen with extended walking, standing, or rising from a seated position.
- Localized Sensations – Some individuals describe the discomfort as a nail-like or pea-sized pressure under the heel.
Without proper management and intervention, symptoms may gradually intensify over time.
Heel Spurs and Their Connection to Plantar Fasciitis
Heel spurs, also known as osteophytes, may develop due to prolonged strain or inflammation of soft tissues such as tendons and ligaments. These bony growths form in response to continuous stress on the heel bone, particularly at the plantar fascia’s attachment site.
Types of Heel Spurs:
- Achilles Heel Spurs – Form at the back of the heel, often linked to Achilles tendon strain.
- Calcaneal Spurs (Plantar Fascia Spurs) – Develop at the bottom of the heel, where the plantar fascia connects to the heel bone.
Common Signs of Heel Spurs
While heel spurs may not always cause noticeable symptoms, some individuals may experience:
- Discomfort During Steps – A sharp, nail-like sensation upon applying pressure to the heel.
- Morning Discomfort – Symptoms often feel more intense after rest, particularly during the first steps of the day.
- Progressive Symptoms – While discomfort may temporarily ease after walking, it can become more persistent over time.
Importance of Comprehensive Assessment for Plantar Fasciitis and Heel Spurs
Addressing heel discomfort and plantar fasciitis involves more than just symptom relief. A thorough assessment of the foot’s structure, movement patterns, and contributing factors is essential in creating an productive care plan. Early intervention may help manage symptoms and facilitate long-term recovery.
Understanding the Causes of Plantar Fasciitis
Plantar fasciitis is commonly caused by excess strain or repetitive stress on the plantar fascia. This connective tissue plays a key role in absorbing shock and managing the foot’s arch during movement. While the exact cause may vary, several contributing factors are frequently associated with this condition.

Key Contributing Factors:
- Repetitive Strain from High-Impact Activities – Running, jumping, and trekking may place excessive stress on the fascia.
- Inadequate Footwear – Wearing shoes that lack proper arch alignment or cushioning can increase strain on the foot.
- Overuse and Prolonged Standing – Excessive weight-bearing activities may cause micro-tears in the plantar fascia.
- Natural Wear and Tear – Over time, cumulative strain on the fascia reduces its ability to absorb impact, leading to irritation.
Under normal conditions, the plantar fascia functions like a shock-absorbing bowstring. However, when tension and pressure exceed its capacity, micro-tears may develop, leading to inflammation and discomfort.
Recognizing Symptoms of Plantar Fasciitis
Plantar fasciitis often presents with gradual, persistent discomfort in the heel or sole of the foot, particularly during weight-bearing activities. The intensity and nature of symptoms may vary based on activity level, footwear, and the severity of inflammation.
Common Symptoms of Plantar Fasciitis:
- Heel Discomfort – Discomfort may be localized to the bottom of the foot or heel and may extend toward the arch.
- Morning Stiffness – Sharp sensations are often most noticeable during the first steps after waking up.
- Post-Activity Discomfort – Discomfort may increase after physical activity, sometimes appearing minutes or hours later rather than during movement.
Symptoms can worsen with prolonged standing, walking, or repetitive foot stress, making early recognition and appropriate care essential.
At-Home Indicators of Inflamed or Strained Foot Ligaments, Tendons, and Muscles
While professional assessments provide the most accurate diagnosis, simple at-home observations and movements can offer insight into potential plantar fascia strain.
Home Observations and Movements:
- Arch Assessment:
- High arches may increase strain on the plantar fascia, contributing to heel or foot discomfort.
- Pinpoint Tenderness:
- Tenderness at the bottom of the foot near the heel bone is commonly associated with plantar fasciitis.
- Discomfort along the sides of the heel may suggest a heel spur or a related issue.
- If tenderness is present in multiple areas, it may indicate a combination of contributing factors.
- Flex Test:
- While seated, pull your toes upward while flexing your foot toward your knee.
- Discomfort at the bottom of the foot during this motion may indicate plantar fascia irritation.
- Ankle Mobility Check:
- Limited upward motion of the ankle may suggest tightness or irritation in the plantar fascia or surrounding soft tissues.
If symptoms persist, seeking professional guidance may help identify the root cause and develop a structured recovery approach.
Understanding Heel Spurs and Their Connection to Plantar Fasciitis
Heel spurs are common in individuals with chronic plantar fasciitis, but they are not always the primary cause of discomfort.
Key Facts About Heel Spurs:
- 1 in 10 individuals may develop heel spurs, but only 5% experience discomfort.
- Chronic plantar fasciitis may contribute to spur formation over time due to continuous stress on the heel bone.
- The discomfort associated with plantar fasciitis comes from inflammation of the plantar fascia, not the bone spur itself.
Recognizing early symptoms and adopting preventive measures may help manage discomfort and reduce the likelihood of heel spur formation.
Exercises to Manage Plantar Fasciitis Recovery
Stretching and strengthening exercises play a key role in managing plantar fasciitis by enhancing foot mobility and function. These exercises target the muscles, ligaments, and tendons surrounding the foot arch, helping reduce strain and improve stability.
Stretching Exercises for Plantar Fasciitis and Heel Discomfort
Stretching the plantar fascia and associated muscles can help relieve tension and promote flexibility. A consistent morning routine of gentle stretching may be beneficial, especially before getting out of bed.
Toe Stretch:
- Position: While lying down, gently flex the foot and toes upward.
- Hold Duration: 5-10 seconds per stretch.
- Repetitions: Three sets, gradually increasing intensity in the second set.
- Caution: Avoid overstretching, as this may lead to calf cramping.
Calf Stretch with Towel:
- Position: Place a rolled towel beneath the balls of your feet while keeping your knee straight.
- Movement: Gently pull on the towel to stretch the plantar fascia and calf muscles.
- Hold Duration: 10-20 seconds, repeating as needed.
Strengthening Exercises for Plantar Fasciitis Recovery
Incorporating strength-building exercises following stretching routines may help reinforce foot care and improve muscle engagement.
Curling Towel Exercise:
- Position: Sit in a chair and place a towel flat on the floor.
- Movement: Using your toes, grip, and pull the towel toward you.
- Benefit: Strengthens the intrinsic muscles of the foot and enhances plantar fascia function.
Marble Picking Exercise:
- Position: Sit comfortably and place marbles on the floor.
- Movement: Using only your toes, pick up the marbles and drop them into a cup.
- Benefit: Strengthens the bottom foot muscles, improving overall foot function and stability.
By combining stretching, strengthening, and proper foot care, individuals may enhance plantar fascia function and reduce the risk of recurrence. Seeking professional care when symptoms persist can help ensure a structured, targeted recovery approach tailored to individual needs.
The Benefits of Icing for Plantar Fasciitis Relief
Applying ice therapy after completing plantar fasciitis exercises can help manage inflammation and promote recovery. Using an ice pack or frozen vegetables wrapped in a towel, individuals can apply cold therapy for 10-15 minutes to the affected foot. This method helps reduce swelling and discomfort, particularly after activity. If needed, repeating the icing process every two hours may provide additional relief.
Risk Factors for Plantar Fasciitis and Heel Spurs
While plantar fasciitis may develop without a clear cause, certain risk factors can increase the likelihood of experiencing foot and heel discomfort.
1. High-Impact Activities: Participating in activities that involve repetitive stress on the heel and plantar fascia may increase the risk of irritation or injury. Some of these activities include:
- Long-distance running
- Jumping exercises such as skipping
- Ballet dancing or aerobic workouts
2. Foot Mechanics and Structure: Individuals with flat feet or high arches may experience uneven weight distribution, placing additional strain on the plantar fascia. This imbalance can increase the risk of heel spurs and foot discomfort.
3. Occupational Factors: Jobs requiring prolonged standing or walking on hard surfaces can contribute to repetitive foot strain. Certain professions, such as teaching, factory work, or retail jobs, may lead to increased stress on the plantar fascia, elevating the risk of developing heel-related concerns.
Home Care for Foot and Heel Discomfort
A structured home care routine may help individuals manage foot and heel discomfort, including plantar fasciitis and heel spurs. Implementing simple self-care techniques can promote recovery, and most individuals notice improvements within approximately ten weeks.
Key Home Care Steps:
- Rest – Reducing or modifying activities that aggravate discomfort can help minimize inflammation and help healing.
- Ice Therapy – Applying ice 2-3 times daily, especially after stretching exercises, may assist in controlling swelling and irritation. To prevent ice burns, the ice pack should always be wrapped in a towel, and each session should be limited to 15 minutes, with a two-hour gap between applications.
- Anti-Inflammatory Medications (If Prescribed): – Non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin or naproxen may provide temporary relief. However, these medications should only be used under medical guidance, and prolonged use beyond two weeks is generally not recommended unless advised by a healthcare professional.
- Stretching Exercises – Incorporating daily foot and calf stretches, particularly after waking up and before engaging in activity, may help relieve tension in the plantar fascia and improve flexibility.
Conservative Approaches for Foot and Heel Discomfort
Many individuals experiencing foot and heel discomfort find relief through non-invasive care methods rather than surgical procedures or injections.
Plantar fasciitis is primarily a mechanical issue, resulting from stress and strain on the plantar fascia. While medications and injections may provide temporary symptom relief, they do not address the root cause of the condition.
A comprehensive, non-surgical approach is often the most integrative method for long-term relief.
How CSC Assist Recovery from Plantar Fasciitis
At Chiropractic Specialty Center® (CSC), a personalized, evidence-based care approach is provided for individuals experiencing plantar fasciitis and heel discomfort. A collaborative team of chiropractors and physiotherapists works together to:
- Assess the underlying causes of discomfort through a detailed evaluation.
- Develop targeted recovery plans that promote natural foot movement and alignment.
- Incorporate rehabilitation-focused techniques, such as shockwave therapy, laser therapy, and physiotherapy-based foot strengthening methods.
This integrative approach has been beneficial for individuals who have not responded well to steroid injections or surgical interventions. By addressing the root causes of plantar fasciitis, individuals may achieve better long-term results while minimizing the risk of recurring symptoms.
Foot Care for Heel Spurs and Plantar Fasciitis
At Chiropractic Specialty Center® (CSC), a comprehensive, non-invasive approach is provided to help individuals experiencing foot and heel conditions such as heel spurs and plantar fasciitis. By combining chiropractic techniques with clinical physiotherapy, the focus is placed on addressing the root causes of discomfort while promoting long-term foot health.
CSC’s Approach to Foot Discomfort Management
CSC’s clinical teams, consisting of experienced chiropractors and physiotherapists, work together to develop personalized care strategies that are both gentle and non-invasive. A structured rehabilitation program may include:
- Manual Physiotherapy – Targeted at soft tissue imbalances and tissue recovery.
- Ultrasound Therapy – Used to help healing and reduce inflammation.
- Shockwave Therapy (ESWT) – Helps break down scar tissue and adhesions.
- High-Intensity Laser Therapy (HILT) – Helps tissue repair while addressing discomfort.
- Interferential Current Therapy (ICT) – A method used to help manage muscle function and foot mobility.
By integrating modern rehabilitation techniques, CSC provides targeted strategies for managing foot-related concerns.
An Integrative and Targeted Approach for Better Results
Unlike conventional care approaches, CSC combines chiropractic care with physiotherapy-based techniques to create a structured, holistic care plan for foot discomfort.
One of the key technologies used in structured foot rehabilitation includes Shockwave Therapy (ESWT), which has been shown to manage tissue function when used alongside manual therapy, chiropractic adjustments, and physiotherapy-based rehabilitation techniques.
While shockwave therapy alone may not be sufficient for managing plantar fasciitis or heel spurs, it plays a valuable role in a comprehensive recovery strategy. By combining multiple rehabilitation techniques, individuals may experience more efficient, long-term relief.
Considering Surgery for Plantar Fasciitis or Heel Spurs

Surgical intervention is typically reserved as a last option after all non-surgical approaches have been attempted for at least 12 weeks. In cases where structured rehabilitation strategies have not provided relief, a surgical consultation may be recommended by a qualified specialist. However, surgery is generally viewed as a final measure when all other conservative approaches have been exhausted.
Common Surgical Procedure for Plantar Fasciitis
One of the most widely performed procedures for plantar fasciitis is gastrocnemius recession, a technique designed to lengthen the calf muscle to improve ankle mobility. This procedure may be performed using an open incision technique or a minimally invasive method with an endoscope (small camera).
Risks and Limitations of Surgery
While some individuals may experience temporary relief from surgical intervention, results are not always long-lasting. Many individuals report recurring discomfort within six months, and in certain cases, symptoms may return even sooner.
Potential Risks of Plantar Fasciitis Surgery:
- Infection at the surgical site.
- Restricted ankle mobility leading to decreased movement in the foot or toes.
- Scar tissue formation which may impact nerve function.
- Chronic stiffness and post-surgical discomfort.
Given these potential complications, many individuals explore non-surgical rehabilitation options before considering surgical intervention. A structured, evidence-based approach to foot recovery may provide long-term benefits while minimizing risks associated with invasive procedures.
Non-Surgical Alternatives for Foot and Heel Discomfort
At Chiropractic Specialty Center® (CSC), a non-invasive, holistic approach is used to help individuals experiencing plantar fasciitis and heel spurs. By focusing on addressing the root causes of discomfort rather than relying on injections or surgical procedures, the goal is to provide long-term relief while enhancing foot function and mobility.
Many individuals experience significant improvements through targeted chiropractic care, physiotherapy-based rehabilitation, and modern therapy technologies designed to manage tissue recovery and reduce discomfort.
CSC’s Approach to Foot Health and Recovery
CSC provides structured, non-invasive care for individuals with foot and heel-related concerns through a collaborative approach involving chiropractors and physiotherapists. This ensures that each individual receives personalized care tailored to their specific condition.
Comprehensive Foot Assessments
Before beginning care, individuals undergo a detailed evaluation conducted by a research-based clinical chiropractor. The assessment, combined with insights from physiotherapists, helps develop a targeted care plan designed to address underlying biomechanical imbalances and improve overall foot function.
Non-Invasive Care for Foot and Heel Conditions
CSC incorporates a wide range of techniques to promote natural recovery and manage foot stability. Some of these methods include:
- Manual Therapy – Includes soft tissue mobilization, trigger point therapy, myofascial release, and joint mobilizations.
- Physiotherapy Modalities – Incorporates ultrasound therapy, shockwave therapy, high-intensity laser therapy (HILT), and interferential current therapy (ICT) to enhance circulation and tissue function.
- Chiropractic Adjustments – Designed to restore proper foot and spinal alignment, helping to improve movement and function.
As part of a comprehensive rehabilitation program, nutritional recommendations, orthotics, and proper footwear selection may also be advised. Custom or over-the-counter arch helps (orthotics) and soft silicone heel pads may help reduce excess pressure on the plantar fascia, providing additional foot care.
Author: Yama Zafer, D.C. – Plantar Fasciitis: Symptoms, Causes & Foot Care
A brief info about the author: Yama Zafer, D.C., educational background in physiotherapy and chiropractic, graduated from Cleveland Chiropractic University in Kansas City, and has spent nearly 3 decades in physiotherapy and chiropractic. Read more about Y. Zafer on his official bio page.
Peer-Reviewed References
- Riddle DL, Schappert SM. Epidemiology of plantar fasciitis. J Am Podiatr Med Assoc. 2004;94(2):178–183.
- DiGiovanni BF, Nawoczenski DA, et al. Plantar fasciitis and calf tightness. J Bone Joint Surg Am. 2003;85(8):1430–1439.
- Sullivan J, et al. The use of night splints in plantar fasciitis. J Orthop Sports Phys Ther. 1999;29(7):413–420.
- Pfeffer GB, et al. Effectiveness of custom orthotics. J Bone Joint Surg Am. 1999;81(2):72–78.
- Martin RL, Irrgang JJ. Foot and ankle examination techniques. Phys Ther. 1999;79(6):585–599.
- Cotchett MP, et al. Stretching programs for plantar fasciitis. BMJ Sports Med. 2014;48(2):e1.
- Rathleff MS, et al. Foot strengthening in plantar fasciitis care. Scand J Med Sci Sports. 2015;25(3):e292–e300.
Last Updated
Last Updated: June 10, 2025 – Plantar Fasciitis Guide for Foot & Heel Care
Contact the Nearest Chiropractic Specialty Center
7 Top FAQs on Plantar Fasciitis That You Should Read
Plantar fasciitis occurs when the plantar fascia, the thick band of connective tissue running along the bottom of the foot, becomes inflamed or strained. Common causes include prolonged standing, improper footwear, excessive foot stress, or high-impact activities.
Symptoms often include:
– Discomfort near the heel.
– Sharp sensations during the first steps in the morning.
– Tightness in the arch or bottom of the foot, particularly after prolonged activity.
Certain groups may be more prone to plantar fasciitis, including:
– Individuals with jobs requiring prolonged standing, such as teachers and factory workers.
– Athletes or individuals engaging in repetitive high-impact activities.
– People with flat feet, high arches, or poorly cushioned footwear.
– Individuals who are overweight, as additional body weight places greater stress on the plantar fascia.
Non-invasive approaches may include:
– Daily stretching exercises targeting the plantar fascia and calf muscles.
– Using proper footwear with arch support helps to maintain healthy foot mechanics.
– Physiotherapy and chiropractic care for foot and spinal alignment.
– Integrated therapy techniques such as ultrasound and shockwave therapy.
Yes, maintaining good foot mechanics can reduce the risk of developing plantar fasciitis. Strategies include:
– Wearing properly fitted, supportive footwear.
– Engaging in strengthening exercises to improve foot stability.
– Avoiding repetitive, high-impact activities that place excess strain on the foot.
Yes, several at-home strategies can help manage symptoms, including:
– Applying ice to the affected area to reduce inflammation.
– Stretching the plantar fascia daily to improve flexibility.
– Using a tennis ball or foam roller under the foot to ease tension.
– Reducing excessive foot strain by modifying activity levels.
If discomfort:
– Persists for more than a few weeks.
– Worsens with activity.
– Interferes with daily activities.
Consulting a qualified healthcare provider for a structured care plan may help support long-term foot health and mobility.
A Non-Surgical, Long-Term Approach to Foot Health
At Chiropractic Specialty Center® (CSC), a comprehensive, evidence-based approach is used to address foot and heel concerns without requiring surgery. By integrating physiotherapy, chiropractic care, and modern rehabilitation techniques, CSC provides a structured, patient-centered recovery plan that helps achieve optimal foot function and mobility.

I have plantar fasciitis for 1 year in my left foot. WHat can be done about this?
Dear Ariff,
Our centers have the best therapy options for Plantar Fascitis. Best of all, the care you get can fix and repair the damage without injections or surgery. Please call our center at 03 2093 1000 for locations and appointment. I hope this helped.
Do you treat degenerative disc desease as well?
Dear Zuhaila,
Thanks for posting a comment. Yes, we treat degenerative disc disease! In adddition to Degenerative Disc Disease , as well as other spine and joints related conditions thorough chiropractic and physiotherapy. You can call our main center on 03 2093 1000 for more information about our locations and services.