Frozen Shoulder Care in Kuala Lumpur
Frozen shoulder, also known as adhesive capsulitis, is characterized by progressive stiffness and restricted movement in the shoulder joint. This condition may result from structural adaptations within the joint capsule or soft tissue influences such as rotator cuff changes or bursitis. Early recognition and structured, non-invasive strategies can help manage mobility and prevent long-term movement limitations.
A comprehensive care approach focuses on improving joint mechanics, soft tissue flexibility, and postural alignment. Research recommends the use of chiropractic and physiotherapy-based interventions, including gentle manual techniques, neuromuscular stimulation, and rehabilitation technologies such as shockwave-assisted mobility help. Addressing contributing factors such as ligament thickening, joint capsule adhesions, and muscular imbalances can help restore shoulder function while minimizing unnecessary strain.
Distinguishing between primary adhesive capsulitis (linked to systemic factors) and secondary adhesive capsulitis (resulting from musculoskeletal adaptations) is essential for tailoring efficient care strategies. Magnetic Resonance Imaging (MRI) is often recommended for assessing joint capsule integrity, soft tissue structures, and early degenerative changes. Evidence highlights the importance of early intervention and structured movement programs to promote shoulder mobility while reducing the risk of progressive stiffness.
This article underscores the benefits of non-invasive methods, integrating chiropractic care, physiotherapy, and rehabilitation technology for shoulder assistance. A well-structured, patient-centered approach can enhance recovery outcomes, reduce reliance on invasive interventions, and manage long-term joint mobility. By identifying and addressing underlying causes, individuals can achieve optimal shoulder function through targeted, evidence-based strategies.
Key Takeaways for Managing Frozen Shoulder
- Identify the Underlying Cause: Understanding whether your frozen shoulder is due to systemic factors or musculoskeletal adaptations is crucial for effective management.
- Seek Non-Invasive Care: Opt for treatments that combine chiropractic adjustments, physiotherapy, and rehabilitation exercises to address the issue holistically.
- Implement Preventative Measures: Incorporate ergonomic practices and regular exercises into your routine to prevent recurrence and maintain shoulder health.
Contact Us for Personalized Frozen Shoulder Care
If you’re experiencing symptoms of frozen shoulder, our team at Chiropractic Specialty Center® in Kuala Lumpur is here to assist. We provide non-invasive care plans tailored to your needs, focusing on safety and effectiveness. Reach out to us today to schedule a consultation and learn more about how we can support your shoulder health. Contact Us
Frozen Shoulder and Adhesive Capsulitis: Causes and Management Strategies
Frozen shoulder, also known as adhesive capsulitis, is a condition characterized by stiffness and restricted movement in the shoulder joint. In its early stages, individuals may experience limited mobility, which can gradually progress if left unaddressed.
Non-invasive strategies focusing on joint flexibility, muscular balance, and underlying structural concerns may help comfort shoulder mobility. The following sections outline common causes of shoulder discomfort and key contributors to frozen shoulder.
What Contributes to Frozen Shoulder and Shoulder Stiffness?
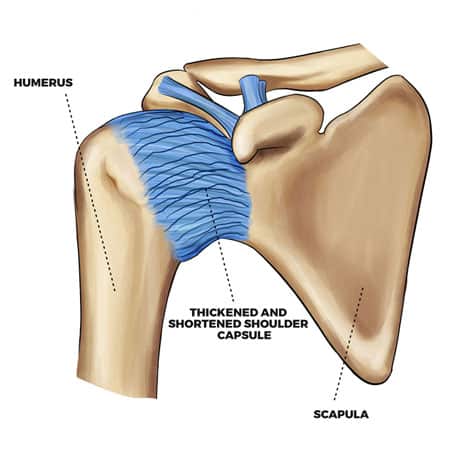
Frozen shoulder occurs when the soft tissues surrounding the shoulder joint undergo structural changes that limit movement. Over time, the joint capsule may thicken, restricting flexibility.
Common Contributing Factors:
- Repetitive Shoulder Strain: Repeated shoulder movements may place stress on muscles and tendons.
- Prolonged Immobility: Reduced shoulder use following injury or surgery may contribute to joint stiffness.
- Systemic Influences: Some metabolic or circulatory conditions have been linked to shoulder mobility adaptations.
Common Structural Influences on Shoulder Mobility
Shoulder mobility concerns may stem from musculoskeletal adaptations, including:
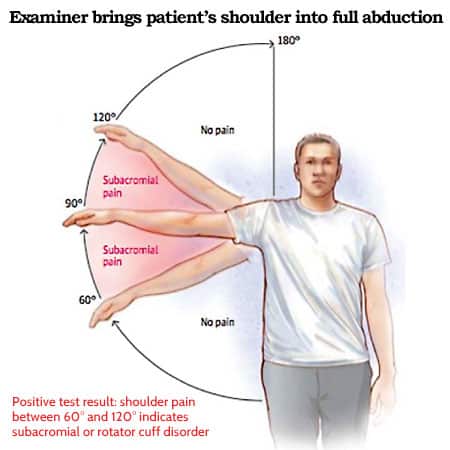
- Rotator Cuff Sensitivity: Structural changes affecting rotator cuff tendons may influence movement.
- Shoulder Impingement: Compression of soft tissues within the joint may contribute to restricted mobility.
- Thoracic Outlet Influence: Sensitivity in the upper chest region may extend to the shoulder.
- Spinal Function: Changes in spinal mobility or nerve pathways may influence shoulder function.
Structured Strategies for Shoulder Mobility Comfort
A well-rounded approach that considers joint mechanics, soft tissue flexibility, and postural influences may help restore shoulder mobility.
Common Non-Invasive Strategies:
- Manual Techniques: Gentle methods to comfort soft tissue flexibility and joint mobility.
- Technology-Assisted Approaches: Rehabilitation technology helping tissue recovery and circulation.
- Postural and Lifestyle Adjustments: Ergonomic modifications and structured movement plans to maintain long-term mobility.
Early intervention is essential for preventing progressive stiffness and maintaining optimal shoulder function.
Understanding the Differences Between Adhesive Capsulitis and Frozen Shoulder Syndrome (FSS)
Although adhesive capsulitis and frozen shoulder syndrome (FSS) share similar characteristics, they differ in their underlying causes.
Key Differences:
- Adhesive Capsulitis: Primarily involves structural changes within the joint capsule.
- Frozen Shoulder Syndrome (FSS): Typically results from soft tissue influences, such as muscle or tendon adaptations.
Understanding these distinctions ensures that shoulder mobility strategies are directed toward the underlying factors affecting movement.
What Contributes to Adhesive Capsulitis?
Adhesive capsulitis is commonly linked to joint capsule inflammation and structural thickening. While the exact cause remains debated, several factors may contribute.
Common Contributors to Adhesive Capsulitis:
- Systemic Influences: Some research suggests a connection between joint inflammation and immune function.
- Capsular Adaptations: Structural changes in the shoulder capsule may reduce flexibility.
- Soft Tissue Influence: Muscular or ligamentous adaptations near the shoulder may contribute to movement restrictions.
Breaking Down the Terminology
To better understand adhesive capsulitis, analyzing its components can provide clarity:
- Capsulitis: Refers to joint capsule inflammation, which may influence mobility.
- Adhesive: Describes the sticking or binding of joint structures, contributing to restricted movement.
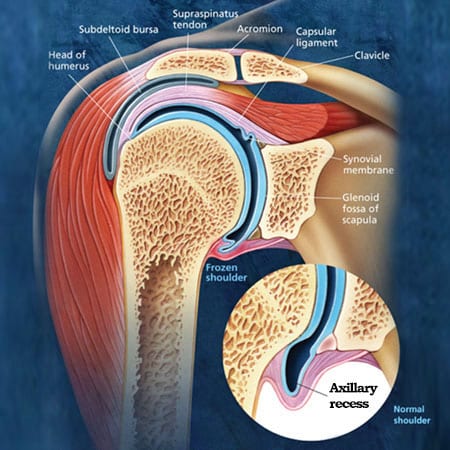
In primary adhesive capsulitis, changes occur within the joint capsule. In secondary adhesive capsulitis, movement restrictions may result from surrounding tissue adaptations, such as rotator cuff changes or bursitis.
A structured, non-invasive approach that focuses on mobility, postural alignment, and joint function may help assist shouldermovement and long-term flexibility.
Distinguishing Between Primary and Secondary Adhesive Capsulitis
1. Primary Adhesive Capsulitis:
- Develops within the shoulder joint capsule, leading to progressive stiffness.
- Associated with joint-specific changes and structural degeneration.
- May have links to inflammatory or systemic factors affecting joint mobility.
2. Secondary Adhesive Capsulitis:
- Results from soft tissue injuries or inflammation, including muscles, tendons, or bursae.
- Commonly associated with rotator cuff injuries or shoulder bursitis.
Understanding whether shoulder stiffness is related to joint capsule changes or surrounding soft tissue influences helps determine the most efficient non-invasive management strategies.
The Influence of Ligaments in Shoulder Mobility
The shoulder joint capsule consists of soft tissues and ligaments that comfort joint stability and flexibility. The capsule contains synovial fluid, which helps nourish cartilage and connective tissues within the joint.
Effects of Ligament Changes on Shoulder Function:
- Structural Adaptations: Repetitive strain or trauma may contribute to ligament thickening (hypertrophy).
- Adhesion Formation: Thickened ligaments may develop fibrotic adhesions, reducing joint flexibility.
- Reduced Synovial Fluid Production: Changes in the capsule may influence joint lubrication and movement.
Potential Outcomes of Structural Ligament Changes:
- Restricted shoulder movement.
- Progressive joint stiffness.
- Challenges in daily activities such as lifting, brushing hair, or reaching overhead.
Recognizing Common Symptoms of Adhesive Capsulitis
Frozen shoulder is often identified by a gradual reduction in joint mobility and increasing stiffness.
Common Symptoms Include:
- Limited Motion:
- Difficulty with overhead movements or across-the-body actions.
- Reduced rotational mobility, especially in chronic cases.
- Discomfort:
- Sensitivity during movement or at rest.
- Sensations that may become more noticeable at night.
- Progressive Stiffness:
- Shoulder movement becomes increasingly restricted over time.
- Prolonged immobility may lead to near-complete loss of movement.
- Potential Contributing Factors:
- Spinal influences such as neck or upper back mobility adaptations.
- Systemic influences, including metabolic or circulatory conditions.
- Post-surgical adaptations following shoulder procedures.
How the Shoulder Joint System Assists Mobility

The shoulder is one of the most mobile regions in the body, allowing a wide range of movement due to its structural design. It consists of multiple joints that function together.
Four Main Shoulder Joints:
- Glenohumeral Joint:
- Primary ball-and-socket articulation between the humerus and scapula.
- Responsible for the majority of shoulder movement.
- Acromioclavicular (AC) Joint:
- Connects the clavicle and acromion, playing a role in lifting and overhead motions.
- Sternoclavicular Joint:
- Links the sternum and clavicle, providing stability.
- Facilitates shoulder elevation and retraction.
- Scapulothoracic Joint:
- A functional articulation where the scapula glides over the ribcage.
- Essential for coordinated shoulder movement.
Types of Adhesive Capsulitis and Their Distinctions
Frozen shoulder is classified into two primary categories based on its underlying cause.
1. Primary Adhesive Capsulitis:
- May be linked to systemic conditions such as metabolic, circulatory, or neurological factors.
- Reported prevalence in individuals with diabetes is approximately 20%.
- Commonly presents as restricted external rotation in early stages.
2. Secondary Adhesive Capsulitis (Frozen Shoulder Syndrome – FSS):
- Develops due to localized shoulder injuries, such as rotator cuff strain or bursitis.
- Frequently results from overuse, trauma, or degenerative changes.
- Early symptoms often include reduced internal rotation, differentiating it from primary adhesive capsulitis.
A structured, non-invasive approach focusing on joint mobility, soft tissue flexibility, and postural comfort can help improve shoulder function and restore movement.
Understanding the Causes of Primary Adhesive Capsulitis

Primary adhesive capsulitis is often linked to systemic health conditions that may influence shoulder joint function. These conditions can contribute to inflammatory responses or capsular adaptations, leading to progressive stiffness and mobility limitations.
Common Factors Associated with Primary Adhesive Capsulitis:
- Autoimmune Conditions: Some immune-related conditions may contribute to joint inflammation.
- Metabolic Influences: Individuals with diabetes have an increased likelihood of developing shoulder mobility adaptations.
- Circulatory Health: Cardiovascular factors may influence joint capsule flexibility.
- Neurological Conditions: Stroke, Parkinson’s disease, and other nerve-related conditions may affect shoulder movement.
- Endocrine Function: Thyroid imbalances (hypothyroidism or hyperthyroidism) may play a role in joint mobility adaptations.
- Respiratory Factors: Some chronic respiratory conditions may influence shoulder movement patterns.
- Post-Surgical Factors: Procedures involving the shoulder or upper spine may contribute to capsular stiffness.
Identifying systemic influences is essential for structuring targeted, non-invasive strategies that comfort shoulder mobility and function.
Understanding the Causes of Secondary Adhesive Capsulitis (Frozen Shoulder Syndrome – FSS)

Secondary adhesive capsulitis, also referred to as true frozen shoulder syndrome (FSS), develops due to structural adaptations in the shoulder’s soft tissues. This condition is often associated with rotator cuff changes, joint irritation, or degenerative influences.
Common Contributors to Secondary Adhesive Capsulitis:
- Rotator Cuff Structural Changes:
- The supraspinatus tendon, which attaches to the humerus, is prone to repetitive strain.
- Structural adaptations may develop near the tendon’s attachment point, influencing mobility.
- Bursitis:
- Inflammation of the bursa (fluid-filled sac) within the shoulder may contribute to reduced movement.
- Tendon Sensitivity:
- Repetitive strain or tendon irritation may influence shoulder flexibility.
- Bone Spurs:
- Structural changes near the acromioclavicular (AC) joint may influence rotator cuff movement.
The Role of Rotator Cuff Muscles in Shoulder Function
The rotator cuff consists of four primary muscles that help shoulder movement and joint stability:
- Supraspinatus: Assists in lifting the arm.
- Infraspinatus: Helps external rotation of the shoulder.
- Teres Minor: Assists with external rotation.
- Subscapularis: Facilitates internal rotation of the shoulder.
Among these, the supraspinatus muscle and tendon are most frequently affected by structural changes. Adaptations near the tendon attachment at the humerus may influence shoulder mobility.
Distinguishing Between Primary and Secondary Adhesive Capsulitis

Although primary adhesive capsulitis and secondary adhesive capsulitis (FSS) share similar mobility limitations, their causes and clinical patterns differ.
Primary Adhesive Capsulitis:
- Linked to systemic factors such as metabolic, circulatory, or neurological conditions.
- Often involves difficulty with external rotation due to capsular changes.
- Both active and passive movement are restricted.
Secondary Adhesive Capsulitis (FSS):
- Results from localized musculoskeletal changes such as rotator cuff strain or bursitis.
- Individuals commonly experience difficulty with internal rotation and passive abduction.
- A defining feature is reduced passive mobility, even when assisted movement is attempted.
By identifying whether shoulder limitations are related to systemic factors or musculoskeletal adaptations, a structured, non-invasive approach can be developed to manage recovery and improve mobility.
MRI as a Preferred Imaging Method for Shoulder Assessment
Magnetic Resonance Imaging (MRI) is a highly efficient imaging method for distinguishing primary adhesive capsulitis from secondary adhesive capsulitis. It provides detailed visualization of the rotator cuff tendons, bursa, joint capsule, and surrounding structures, helping to identify contributing factors affecting shoulder mobility.
By determining whether the shoulder capsule (primary adhesive capsulitis) or surrounding soft tissues (secondary adhesive capsulitis) are involved, structured, non-invasive care strategies can be implemented promptly to comfort mobility and recovery.
MRI: The Recommended Imaging Method for Shoulder Conditions
While X-rays and ultrasound can provide insights into joint and soft tissue structure, MRI remains the preferred method for evaluating shoulder mobility concerns.
Why MRI is Preferred for Shoulder Assessment:
- Soft Tissue Imaging: Detects muscle, tendon, and ligament structures in detail.
- Joint Capsule and Cartilage Assessment: Provides clear visualization of joint surfaces and surrounding soft tissues.
- Structural Analysis: Identifies bone spurs, capsule changes, and early signs of degenerative influences.
For individuals experiencing persistent shoulder mobility limitations, consulting a healthcare professional to determine whether an MRI assessment is necessary may help a well-structured care plan.
At-Home Strategies for Assisting Shoulder Mobility
Managing shoulder mobility concerns at home involves protecting the joint, maintaining flexibility, and reducing stress on soft tissues.
Recommended Home Strategies:
- Minimize Excessive Strain:
- Avoiding repetitive overhead movements and sudden shoulder strain may help manage recovery.
- Some individuals may find shoulder slings beneficial in minimizing excessive movement during certain activities.
- Cold Applications for Localized Irritation:
- Applying a cloth-wrapped ice pack for 15 minutes every 2-3 hours may help manage localized irritation.
- Ice should never be applied directly to the skin, and icing sessions should be limited to under 20 minutes with at least a 1-hour gap between applications.
- Gentle Mobility Exercises:
- Performing controlled, discomfort-free arm movements may help maintain joint flexibility.
- Movements should be gentle and within a comfortable range, followed by cold application if needed.
- Professional Assessment:
- While home strategies may provide temporary alleviation, a professional evaluation is essential for structured recovery.
- Addressing shoulder mobility concerns early may help prevent further restrictions in movement.
Non-Invasive Strategies for Shoulder Mobility Care

Both primary and secondary adhesive capsulitis benefit from structured, non-invasive approaches that focus on joint function, soft tissue mobility, and muscular stability.
Common Strategies for Shoulder Care:
- Comprehensive, Non-Invasive Approaches:
- A structured care plan may integrate chiropractic and physiotherapy-based approaches to promote joint mobility and soft tissue function.
- Multi-Modal Care Strategies:
- Manual techniques for targeted mobility, care.
- Rehabilitation technology-assisted approaches, including:
- Shockwave-assisted rehabilitation
- Ultrasound-based mobility helps
- Neuromuscular stimulation techniques
- Soft tissue mobility approaches
- Targeted movement rehabilitation
- Strength and Flexibility Care:
- Shoulder mobility limitations may lead to soft tissue changes over time.
- A structured strengthening and flexibility-focused approach can help maintain joint stability and mobility.
The Importance of Professional Assessment
Seeking structured, professional evaluation is essential for conditions such as adhesive capsulitis to ensure an accurate assessment and a targeted care strategy.
A structured, non-invasive approach can comfort shoulder mobility, minimize discomfort, and reduce the need for invasive interventions such as injections or surgical procedures.
Yama Zafer, D.C. – Frozen Shoulder Care: Non-Invasive Options in Malaysia
Yama Zafer, D.C., with a background in physiotherapy and chiropractic from Cleveland Chiropractic University in Kansas City, has dedicated nearly 30 years to providing non-invasive spine and joint care; read more about Y. Zafer.
Peer-Reviewed References
- Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003;48(3):829-838.Wikipedia
- Diercks RL, Stevens M. Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. J Shoulder Elbow Surg. 2004;13(5):499-502.
- Mertens MG, Meert L, Struyf F, et al. Exercise therapy is effective for improvement in range of motion, function, and pain in patients with frozen shoulder: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2022;103(5):1011-1021.Wikipedia
- Nakandala P, Nanayakkara I, Wadugodapitiya S, Gawarammana I. The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. 2021;34(3):409-418.Wikipedia
- Lädermann A, Piotton S, Abrassart S, et al. Hydrodilatation with corticosteroids is the most effective conservative management for frozen shoulder. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2553-2561.Wikipedia
- Kirker K. Manual therapy and exercise for adhesive capsulitis: a systematic review with meta-analysis. J Man Manip Ther. 2023;31(5):235-245.Wikipedia
- Dimitris C, Biddle M, McLean M, Millar NL. Comparison of treatments for frozen shoulder: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(12):e2029581.
Last Updated
Last updated on June 3, 2025: Frozen Shoulder Care in Kuala Lumpur


Any hope for a frozen shoulder plain?
Dear Linda,
Thanks for posting a comment. Frozen shoulder results from injuries and degenerative changes that occur in the shoulder joints. The shoulder has two main joints: The acromial-clavicular joint (A/C joint) and the glenohumeral joint (the true shoulder joint). Injuries and degenerative changes in these joints and their soft tissues (muscles and ligaments) lead to pain and an inability to move shoulders freely.
Also, patients with a frozen shoulder may have issues in their neck and upper back. Neck pain and upper back pain (pain between the shoulders) are common in frozen shoulder patients as some muscles attach to the neck, upper back, and shoulders.
To recover, you will need care that focuses on the root cause of your pain. As such, a thorough assessment of the shoulder joint and your neck and upper back are needed. Identification of the exact cause of pain is essential to complete recovery. CSC’s clinical team of chiropractors and physiotherapists have the knowledge and skills to assess and provide you with the best holistic treatment. I invite you to call our center at 03 2093 1000 for more information about our shoulder treatment programs.
I hope this helped.
Hi Yama, thank you for your effort in posting the articles on your blog.
On 25/10/23 and 28/10/23, I played badminton. On 29/10/23, I noticed my right collarbone popped out more than my left collarbone. I went to the doctor, and he diagnosed it as stenoclavicular anterior subluxation or dislocation. Most of the pain and swelling are gone, but my shoulder feels stiff sometimes, like some blood flow is incorrect. The doctor didn’t advise surgery due to the risks, and he told me to “live with it”. But it has been draining me mentally as I am afraid to exercise, play badminton again or even reach back for my wallet with my right hand because I would stress the joint. So my questions are: –
1. Are there any chiropractic doctors in your clinics who have successfully brought the raised stenoclavicular joint back down to the same level as the opposite joint?
2. May I know their name and which branch?
I want to fix the joint, ensure both clavicles are optimistically placed, and then take glucosamine and chondroitin supplements to help repair it. I will also go on a one-year upper body exercise regime to rebuild the muscle and tissue I have lost from ageing. I just turned 50. Are there any chiropractors in your clinics with proven experience in successfully restoring anterior stenoclavicular subluxation?
Thanks!
Dear Edwin,
Thank you for reaching out with your concerns about the sternoclavicular (SC) joint subluxation you’ve experienced. This type of joint issue, where the connective tissue is damaged, often results from traumatic events such as intense physical activity, in your case, playing badminton. Understanding and addressing this correctly is crucial to preventing further complications and ensuring a return to your regular activities without pain or mental strain.
A subluxated or dislocated sternoclavicular (SC) joint results when the joint’s connective tissue is damaged. To reposition the sternoclavicular joint without popping out again, you will need targeted and personalized care. But before this can be done, you should have a thorough assessment of the SC joint, the Acromioclavicular (AC) joint, and the shoulder girdle (glenohumeral joint).
The stiffness you mentioned may have resulted from the traumatic event that caused this sternoclavicular subluxation. The traumatic episode that led to the subluxation may also have damaged the SC joints’ cartilage and ligaments, the joint of your first rib, the subclavius muscles, the AC joint, and the shoulder joint, all of which are closely related to the sternoclavicular joint. A sternoclavicular (SC) subluxation can significantly impact the entire shoulder girdle, including the acromioclavicular (AC) joint and the glenohumeral articulation.
Impact on the Acromioclavicular (AC) Joint
The AC joint, located where the clavicle meets the acromion of the scapula, is integral to the upper shoulder’s stability and movement. When the SC joint is subluxated:
• Altered Biomechanics: The clavicle’s position is altered due to the SC subluxation, which can lead to abnormal movement patterns at the AC joint. Since the clavicle serves as a strut between the sternum and scapula, any displacement at the sternum end (SC joint) can affect its scapular end (AC joint).
• Increased Stress: Changes in clavicular alignment increase mechanical stress across the AC joint. This can exacerbate existing conditions like AC joint arthritis or lead to the development of new symptoms, including pain and restricted movement.
• Compensatory Movements: To accommodate the altered position of the clavicle, the scapula may rotate or tilt abnormally, impacting the AC joint’s normal function and possibly leading to degenerative changes over time.
Impact on the Glenohumeral Articulation
The glenohumeral joint, which is the ball-and-socket articulation between the humerus and the glenoid fossa of the scapula, is primarily responsible for the arm’s wide range of motion. A SC subluxation affects this joint by:
• Altered Scapular Positioning: As the SC joint subluxation affects the position of the clavicle and potentially the scapula, it can lead to a condition known as scapular dyskinesis, where the scapula does not move normally. This altered scapular motion can impair glenohumeral rhythm, the coordinated movement between the scapula and humerus, essential for optimal shoulder function.
• Restricted Range of Motion: Changes in the biomechanics of the scapula and clavicle can limit the range of motion at the glenohumeral joint, particularly in overhead or extended movements, leading to stiffness and discomfort.
• Increased Risk of Injury: The glenohumeral joint’s stability is partly reliant on the coordinated action of the surrounding muscles and bones, including the scapula and clavicle. Disruption in this system, such as from a SC subluxation, increases the risk of shoulder injuries, including rotator cuff tears and impingement syndrome, due to the abnormal load and stress on the joint.
Additionally, you may have damaged small muscles under the clavicle, known as the subclavius muscles. The subclavius muscle plays several important roles:
• Stabilization: It helps stabilize the clavicle by anchoring it to the first rib, thus preventing any excessive movement that might disrupt the integrity of the shoulder girdle.
• Depression of the Clavicle: During shoulder movements, it depresses the clavicle to aid in the full range of motion, particularly when the shoulder lifts or rotates.
• Protection: It also acts as a protective buffer for the underlying nerves and blood vessels that pass between the chest and the upper limb.
How the Subclavius Muscle Gets Injured
Injuries to the subclavius muscle can occur but are relatively rare due to its protected position under the clavicle. Possible causes of injury include:
• Direct Trauma: Such as a blow to the clavicle area, which can occur in contact sports or from a fall.
• Repetitive Strain: Activities that involve repetitive shoulder and arm movements, especially overhead activities, can strain the subclavius muscle.
• Severe Shoulder Movements: Sudden, intense movements of the shoulder can stretch or tear the subclavius muscle.
Subclavius Muscle Injury and Sternoclavicular (SC) Joint Issues
Injuries to the subclavius muscle can affect the sternoclavicular joint, where the sternum meets the clavicle. This is primarily due to the muscle’s role in stabilizing and supporting the clavicle:
• Subluxation: Although rare, severe or repetitive trauma to the subclavius muscle can lead to subluxation of the SC joint. This occurs when the support provided by the subclavius is compromised, allowing the clavicle to move out of its normal alignment with the sternum.
• Stiffness: Injury to the subclavius can lead to stiffness in the SC joint by causing inflammation or by compensatory mechanisms where the body restricts movement to prevent pain or further injury.
To conclude, you need a thorough assessment of the sternoclavicular joints, its soft tissues (ligaments), and the subclavius muscle, as well as the AC joint to formulate a targeted treatment plan collaboratively provided by chiropractors and physiotherapists. At CSC we can help with this assessment, chiropractic care as well as physiotherapy and rehabilitation to ensure MMI (Maximum Medical Improvement).
In the past few decades, I have treated several people with similar issues, some of whom I have been able to help. The key to complete recovery is to focus treatment on areas in need. Most importantly, the resolution of injuries is achieved through timely care with appropriate methods. If you would like to be consulted by me or one of the other chiropractors in our office please WhatsApp us at +(6017-269-1873.